Preclinical studies on therapies for CLN1 disease

The lab has worked with Mark Sands, PhD, for many years to develop gene therapy for CLN1 disease. As we have learned more about which regions of the CNS are affected, we have been better able to treat them. This especially includes the spinal cord, which is affected especially severely in CLN1 disease. Increasingly, we are also looking at disease outside the brain and how to treat it (see below). We are also exploring how microglia are affected in this form of NCL, investigating how their biology is compromised and the effects this has for neurons. In addition to gene therapy, we are also working on developing an enzyme replacement therapy for CLN1 disease. This has been first tested in CLN1 mice and then scaled up in CLN1 disease sheep. These were developed by Tom Wishart, PhD, and his team at the Roslin Institute in Scotland. We are also developing a gene therapy strategy in these CLN1 sheep.
Preclinical studies on therapies for CLN2 disease
Although an FDA approved enzyme replacement therapy for CLN2 disease is now available, we are working to better understand how the brain, spinal cord and other tissues are affected in this disorder. This includes investigating the impact of TPP1 deficiency in different cell types via the use of cell type-specific knockout mice and designer receptor exclusively activated by designer drugs (DREADDS). We are also interested in testing other therapies that may be more effective, either by using a different gene therapy study or targeting this to the sites that are most affected (including outside the brain – see below). Our work is revealing how CLN2 is very different to other NCLs (especially CLN1 disease). We have also looked in detail at the seizure phenotypes of CLN2 mice, what cell types cause this and how this may be better treated.
Preclinical studies on therapies for CLN3 disease
We have been working to better understand the effects of CLN3 disease upon the brain and spinal cord. We have looked at how glial biology is compromised and which CNS regions are affected, and used this information to test a range of anti-inflammatory compounds, or how stimulating TFEB may be therapeutic (in collaboration with Marco Sardiello, PhD). A major new area is the impact of CLN3 disease upon the peripheral nervous system and enteric nervous system and their contribution to disease outcome. In addition we are using gene therapy to target these under appreciated, but debilitating effects of disease.
Pathology outside the brain in neuronal ceroid lipofuscinoses
Although most of our attention has been upon the brain and spinal cord, it is becoming more apparent that other tissues and neurons outside the brain are severely impacted by disease in multiple forms of NCL. This includes severe gastrointestinal problems, which we also see in our mouse models, and appear to be associated with severe enteric nervous system (ENS) pathology (work in collaboration with Robert Heuckeroth, CHOP). Batten children —and our mice — also display a range of peripheral nerve phenotypes and we are exploring the basis of this within the motor and sensory components of the peripheral nervous system (PNS), together with Alison Snyder-Warwick, MD. We are currently targeting treatment to the ENS and PNS via gene therapy.
Glial involvement in neuronal ceroid lipofuscinoses
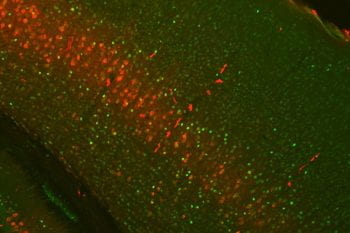
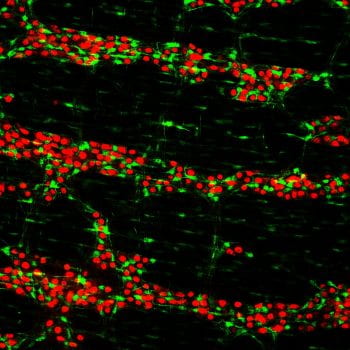
There are up to 13 different forms of neuronal ceroid lipofuscinoses (NCL), each having distinct monogenetic defects in genes encoding proteins in the endo-lysosomal system. However, little is known about how deficiency of each protein causes neurodegenerative phenotypes, which has hampered designing new therapeutical approaches for NCLs.
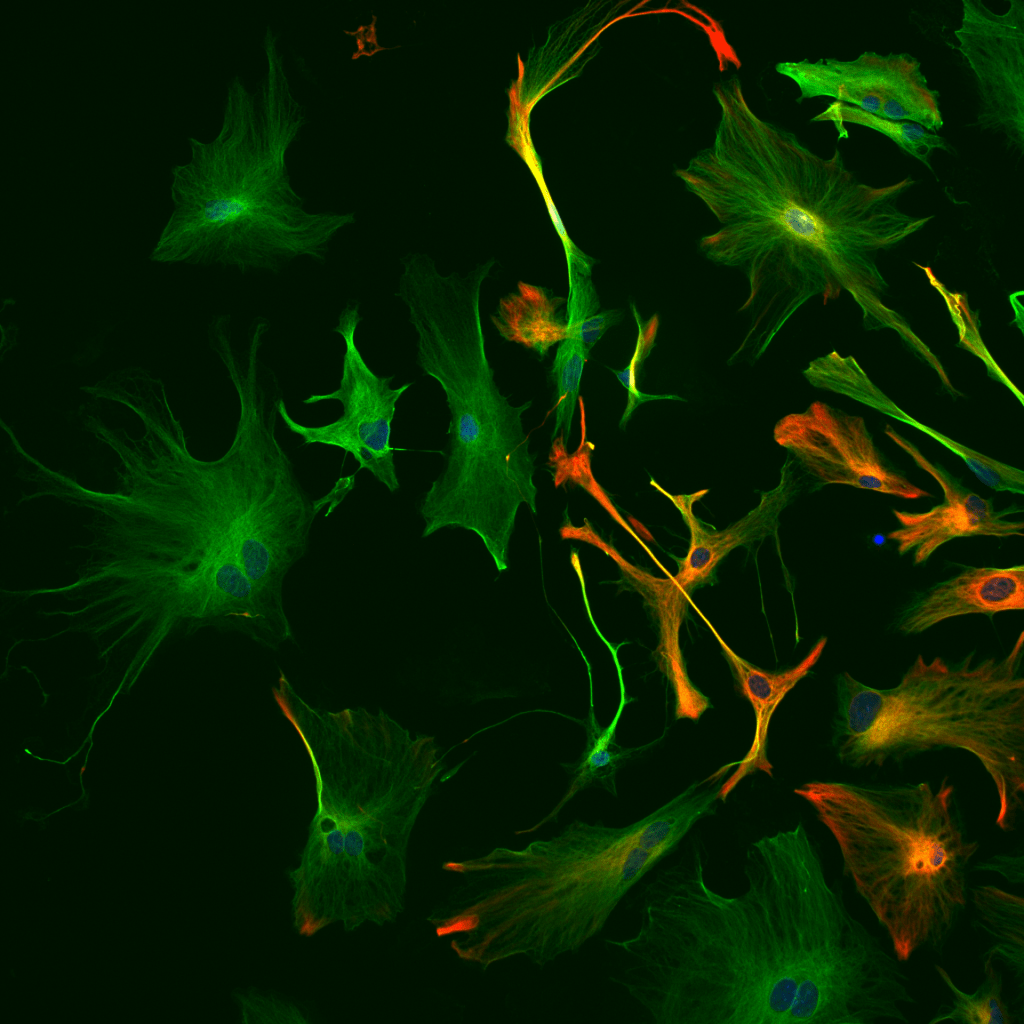
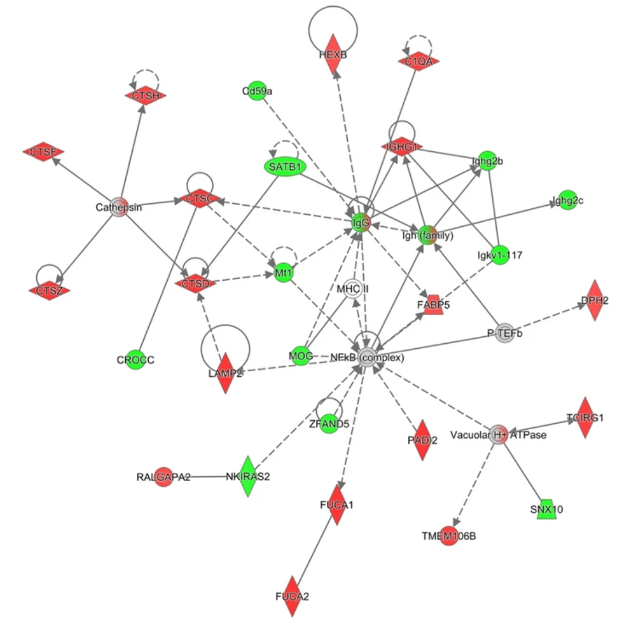
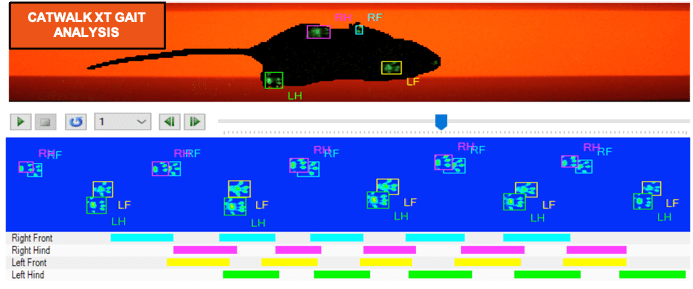
The characterization of animal models of NCLs has revealed glial cells to be adversely affected and actively contribute to disease progression. Employing multiple techniques including transcriptomics, proteomics, primary cell cultures, genetic engineering, histological image analysis, and behavioral studies, we are investigating potential mechanisms by which glia contribute to neuron loss associated NCLs.